Abstract
Objective :This study aims to analyze the clinical features, prognostic characteristics and gene mutations of the primary myelodysplastic syndrome with myelofibrosis (MDS-MF) patients, ultimately to improve the cognition of MDS-MF.
Methods :From January 1, 2013 to February 1, 2020, 417 newly diagnosed primary MDS patients in the first affiliated hospital of Zhejiang University with bone marrow (BM) biopsy examination were included. They were divided into two groups according to whether BM associated with fibrosis (2005 European Myelofibrosis Network criteria), the MDS-MF group(MF grades 1-3)and the MDS without MF group (MDS-MF0).The clinical features, prognosis characteristics and gene alterations were analyzed between the two groups retrospectively.
Results :
① MF was confirmed in 46.3%(193/417)cases of all the MDS patients, of which 66.3%(128/193)were MF-1 , 25.9%(50/193)were MF-2 and 7.8%(15/193) were MF-3 respectively. The proportion of MDS-EB in MDS-MF group was 48.2%(93/193) and significantly higher than in MDS-MF0 group 35.7%(80/224),the difference had statistical significance(P=0.008). However, the occurrence of MF does not differ among the MDS subtypes according to the 2016 WHO classification (P=0.342).
② The clinical features of the two groups had statistically significant differences in the higher number of BM blast cells(P=0.006), higher prevalence of death (P=0.031), higher rate of Leukemic transformation (P<0.001), higher level of serum lactate dehydrogenase (LDH) in the peripheral blood (p<0.001), higher level of β2-microgram in the peripheral blood(p=0.003) and higher level of C-reactive Protein (CRP) in the peripheral blood (P=0.004) in the MDS-MF group than in the MDS-MF0 group. The number of WBC, Hb, PLT and Ferritin at the first diagnosed in our hospital were no difference compared the two groups (All P>0.05). The sex, Age and the IPSS-R score(IPSS-R >3.5 v ≤3.5) were no difference in the two groups (ALL P>0.05).
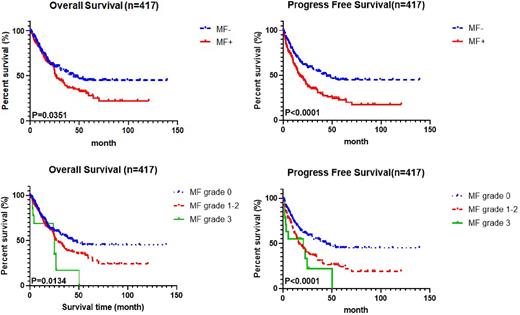
③Compared with MDS-MF0 group, MDS-MF were significantly associated with worse OS(P=0.035) and worse PFS(p<0.001). The median overall survival was 13.20(0.07-90.70) months in MDS-MF group, and was 23.77(0.53-98.97) months in MDS-MF0 group respectively. Subgroup analysis showed that both OS and PFS of either the MDS-MF1-2 group or the MDS-MF 3 group were also significantly worse than those of the MDS-MF0 group(P=0.013 and <0.001 respectively).
④Among all the patients ,337 were finished Next-generation-sequencing (NGS) test, sequencing errors and all known or possible single-nucleotide polymorphisms were excluded. The number of mutations (>2) was more frequently in the MDS-MF, the difference had statical significance(P=0.030). The RNA splicing was more frequently in the MDS-MF than the MDS without MF, the difference also had statical difference(P=0.025). The ratio of U2AF1 mutation occurred in MDS-MF group higher than MDS-MF0 group, the difference had statical significance (P=0.027). There was totally 14.2% (48/337) patients with the mutation of U2AF1, of which 19.7%(29/147) in MDS-MF group and 10.0%(19/190) in MDS-MF0 group.
Conclusion: MDS-MF has unique laboratory and clinical characteristics. MF is an independent risk factor for shorter overall survival (OS) and worse progression-free survival (PFS) in primary MDS. Evaluation of MF is very significant for prognosis judgment in primary MDS. The U2AF1 mutation may be a biomarker related to the occurrence and poor prognosis of MDS-MF. However, the mechanism of U2AF1 in MDS-MF patient needs to be further explored.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal